Did you know your body hosts 40 trillion bacterial cells—outnumbering human cells? This vast ecosystem, called the microbiome, weighs as much as your brain and functions like a hidden organ. It shapes everything from digestion to your immune system.
Research reveals a diverse gut environment supports better health. Imbalances, however, link to conditions like obesity and heart disease. Your diet, lifestyle, and even stress levels directly influence this delicate balance.
Scientists now consider the microbiome a critical player in long-term wellness. By nurturing its diversity, you can boost metabolism, mood, and disease resistance. Ready to unlock its potential?
Key Takeaways
- Your microbiome contains 40 trillion bacterial cells—more than human cells.
- It acts like a vital organ, impacting immunity and metabolism.
- Gut bacteria diversity correlates with better health outcomes.
- Imbalances may contribute to chronic diseases like obesity.
- Diet and lifestyle choices directly affect microbiome health.
What Is the Gut Microbiome?
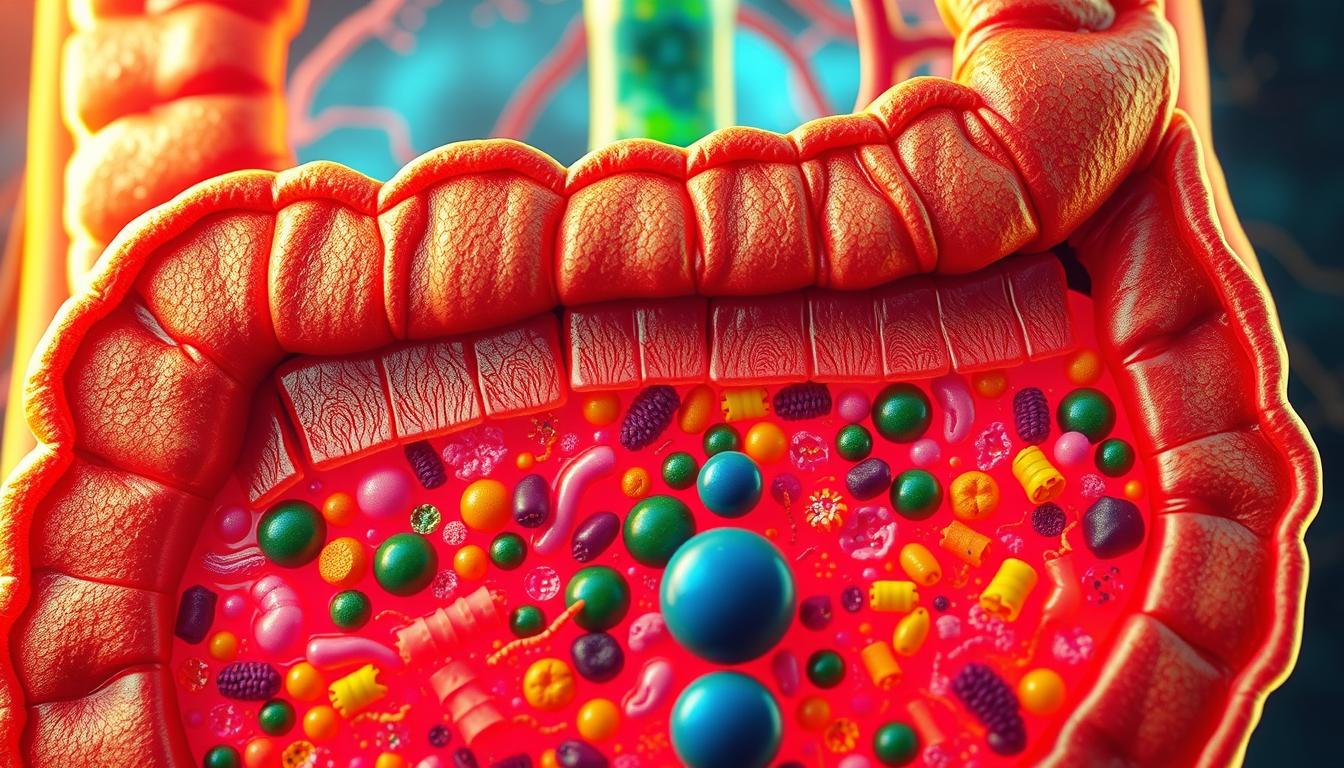
Deep within your digestive tract lies a thriving ecosystem of microscopic life. This community, known as the gut microbiome, primarily resides in the cecum—a pouch at the start of your large intestine. Here, trillions of microorganisms collaborate to keep your body functioning optimally.

Definition and Composition
The gut microbiome includes bacteria (the dominant group), viruses, fungi, and archaea. Over 1,000 bacterial species coexist, such as Bifidobacteria and Lactobacilli, which aid infant digestion and immune development. These types bacteria form a delicate balance, each contributing to nutrient processing.
Role in the Human Body
Microbes engage in cross-feeding—a process where one microorganism’s waste becomes another’s fuel. This synergy ensures efficient digestion and vitamin production. A diverse microbiome also strengthens resilience against pathogens, acting as a shield for your body.
“Microbial diversity in the large intestine is like a fingerprint—unique to each individual and critical for health.”
When this diversity declines, imbalances may arise, linking to health issues. By nurturing your gut microbiome, you support everything from immunity to mental clarity.
Why the Gut Microbiome Is Essential for Your Health
Your gut microbiome isn’t just a passenger—it’s an active partner in your well-being. This complex community of microbes collaborates with your body, influencing everything from nutrient absorption to disease defense.
Symbiotic Relationship with the Body
Your gut bacteria thrive on fiber, breaking it into short-chain fatty acids (SCFAs) like butyrate. These compounds nourish your intestinal lining, lowering pH to block harmful pathogens. In return, your body provides a stable habitat—a true symbiotic relationship.
SCFAs also reduce inflammation and strengthen the gut barrier. Studies show they may protect against conditions like inflammatory bowel disease (IBD). Disruptions, such as antibiotic use, can weaken this balance, leaving your system vulnerable to infections.
Key Functions in Digestion and Immunity
Beyond digestion, your microbiome trains immune cells to distinguish foes from allies. Beneficial bacteria, like Bifidobacteria in infants, even rely on breast milk sugars to flourish—a natural boost for early immunity.
“Gut microbes act as educators, shaping immune responses that last a lifetime.”
When this microbial balance falters (dysbiosis), miscommunication can trigger autoimmune reactions. Prioritizing nutrients that feed good bacteria—think fiber and fermented foods—helps maintain this delicate equilibrium.
How the Gut Microbiome Affects Your Weight
Your weight may hinge on an invisible army of gut bacteria working behind the scenes. Research shows these microbes extract energy from food, influence cravings, and even alter fat storage. When their balance shifts—gut dysbiosis—it can tip the scales toward obesity.
Gut Dysbiosis and Weight Gain
Studies of twins reveal stark differences in microbial species between obese and lean individuals. Harmful bacteria thrive on processed foods, extracting extra calories and triggering cravings for sugar. This creates a cycle of overeating and metabolic slowdown.
Mice transplanted with obese microbiomes gained weight despite identical diet plans. Similarly, humans with low microbial diversity often struggle with insulin resistance. The key? Restoring balance to support healthy metabolism.
Can Probiotics Help Manage Weight?
Probiotics like Lactobacilli show promise in modest weight management. They may reduce cholesterol absorption and curb inflammation linked to fat storage. However, effects vary by strain—highlighting the need for targeted solutions.
“Probiotics aren’t magic bullets, but they can tilt the microbial balance in your favor.”
| Factor | Impact on Weight | Microbial Players |
|---|---|---|
| High-fiber diet | Promotes fat burning | Bifidobacteria |
| Artificial sweeteners | May increase fat storage | Enterobacteriaceae |
| Fermented foods | Supports metabolism | Lactobacilli |
Avoiding artificial sweeteners is critical—they encourage harmful bacteria linked to obesity. Instead, focus on fiber-rich foods to nourish beneficial species and break the cycle of gut dysbiosis.
The Gut Microbiome and Digestive Health
Your digestive health depends heavily on the balance of bacteria gut microbes. When this balance falters, conditions like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD) can emerge. These disorders often stem from dysbiosis—a microbial imbalance that disrupts gut function.
Link to IBS and IBD
Bloating, cramps, and irregular motility signal IBS, frequently tied to low microbial diversity. In bowel disease like IBD, chronic inflammation damages the intestinal lining. Toxins then leak into the bloodstream, triggering immune reactions.
Western diets high in saturated fats worsen IBD symptoms by starving beneficial cells. Studies show Bifidobacteria and Lactobacilli strains can reduce flare-ups by calming gut inflammation.
Preventing Leaky Gut Syndrome
Leaky gut occurs when intestinal gaps widen, allowing harmful particles to escape. Probiotics like Saccharomyces boulardii reinforce tight junctions between cells, sealing these gaps.
- Fiber feeds SCFA producers: These compounds strengthen the gut barrier.
- Avoid NSAIDs and alcohol: They erode the lining and worsen permeability.
“Restoring microbial balance is 80% of the battle in managing digestive disorders.”
Focus on fermented foods and prebiotics to nourish protective bacteria gut communities. This simple shift can shield against inflammatory bowel disease and improve overall digestion.
Heart Health and the Microbiome
Emerging research reveals a surprising link between gut bacteria and cardiovascular wellness. Your microbiome doesn’t just digest food—it produces compounds that directly affect cholesterol levels and artery health. Imbalances may elevate cardiovascular risk, making microbial diversity a key player in prevention.

Impact on Cholesterol and Triglycerides
Certain gut bacteria, like Lactobacilli, help metabolize cholesterol, reducing LDL (the “bad” type). Studies show probiotic strains can lower LDL by 12% when combined with a fiber-rich diet. These microbes convert excess cholesterol into compounds excreted in blood, preventing buildup.
| Dietary Factor | Effect on TMAO | Microbes Involved |
|---|---|---|
| Red meat (high choline) | Increases TMAO | Prevotella, Bacteroides |
| Plant-based foods | Lowers TMAO | Bifidobacteria |
| Fermented dairy | Neutralizes TMAO | Lactobacilli |
TMAO and Cardiovascular Risk
When gut microbes break down choline (found in red meat), they produce TMAO—a compound linked to atherosclerosis. High TMAO levels stiffen arteries and may double heart disease risk. Plant-based diets reduce TMAO by starving the bacteria that produce it.
“TMAO is like rust in a pipe—it accelerates plaque buildup, narrowing arteries over time.”
Probiotics and fiber-rich foods can shift microbial activity away from TMAO production. For lasting heart health, prioritize leafy greens, oats, and fermented foods to nurture protective bacteria.
The Gut-Brain Connection
Your gut and brain communicate constantly through a hidden superhighway. This gut-brain axis, primarily via the vagus nerve, lets bacteria influence mood and cognition. When this system falters, mental health may suffer.
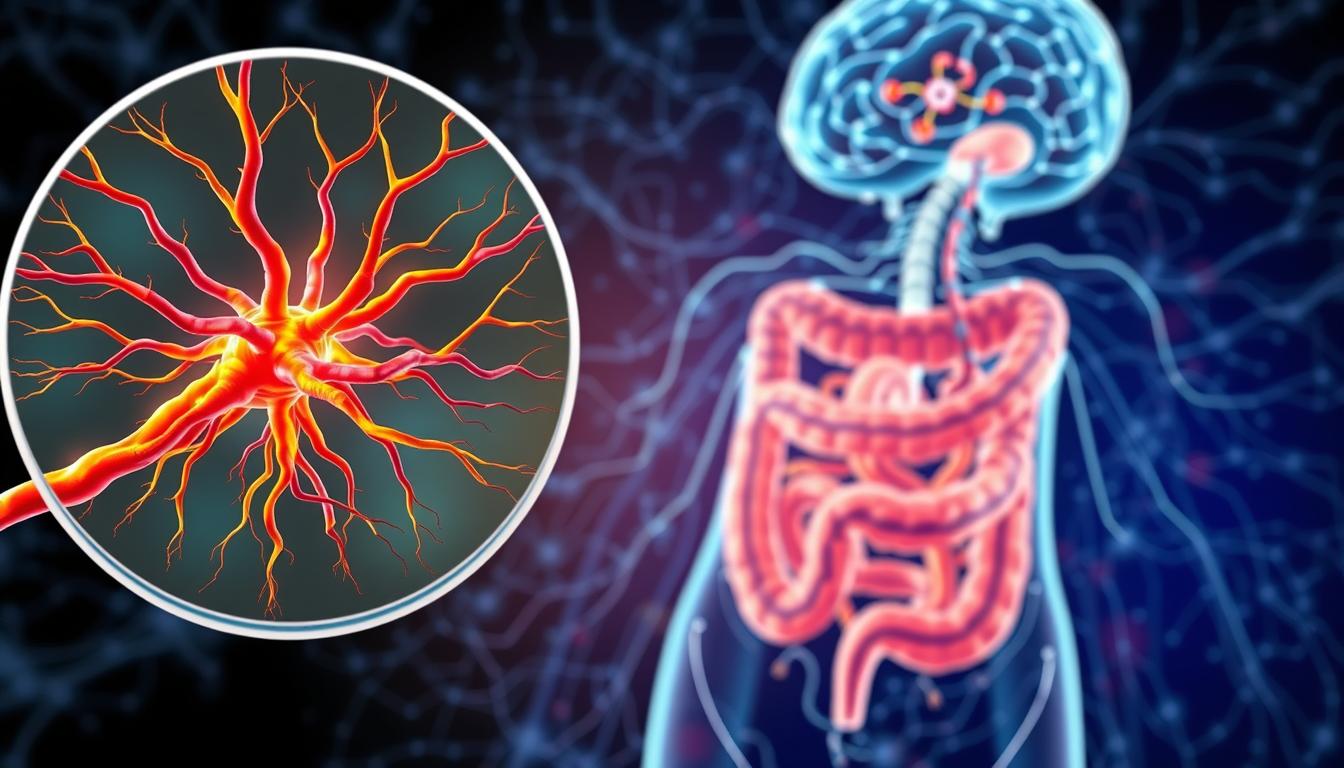
Neurotransmitters and Mental Health
Nearly 90% of serotonin—your happiness chemical—is made in the gut by microbes like Clostridia. Low microbial diversity correlates with depression, as fewer bacteria produce these vital neurotransmitters.
Twin studies reveal distinct microbiome patterns in people with anxiety disorders. Those lacking Bifidobacterium often show higher stress responses. Probiotics like B. longum can lower cortisol by 25%.
“Gut bacteria don’t just digest food—they manufacture the chemicals that dictate how you feel.”
Microbiome’s Role in Stress and Anxiety
Dysbiosis triggers inflammation, weakening the blood-brain barrier. Harmful compounds then leak into the brain, disrupting cells that regulate emotions. Germ-free mice exhibit exaggerated fear responses, mirroring human anxiety.
| Probiotic Strain | Effect on Mental Health | Study Findings |
|---|---|---|
| Bifidobacterium longum | Reduces cortisol | 25% lower stress markers |
| Lactobacillus rhamnosus | Boosts GABA | Calms neural activity |
| Clostridia species | Protects against allergies | Linked to mood stability |
To support this connection, prioritize fermented foods and fiber. They nourish bacteria that keep both your gut and brain in sync.
Signs of an Unhealthy Gut Microbiome
Your gut sends clear signals when its microbial balance is off—learn to recognize them. From bloating to sudden weight shifts, these symptoms often point to dysbiosis. Left unchecked, imbalances may escalate into chronic disease.

Common Symptoms of Dysbiosis
An imbalanced microbiome announces itself in surprising ways:
- Digestive distress: Bloating, diarrhea, or constipation lasting weeks.
- New food intolerances: Sudden reactions to foods like dairy or gluten.
- Unexplained weight changes: Gain or loss without diet shifts.
Slow motility (delayed digestion) can cause SIBO—a bacterial overgrowth in the small intestine. Breath tests detect excess gases like hydrogen, confirming SIBO.
| Symptom | Possible Cause | Action |
|---|---|---|
| Chronic fatigue | Low microbial diversity | Increase prebiotic fiber |
| Recurrent infections | Antibiotics disrupting flora | Probiotic supplements |
| Blood in stool | Inflammation or injury | Seek medical advice |
When to Seek Help
Over-the-counter microbiome tests lack clinical validation. Instead, consult a doctor if you notice:
- Persistent symptoms despite diet changes.
- Blood in stool or severe abdominal pain.
- History of C. difficile after antibiotics.
“Ignoring gut symptoms is like silencing a smoke alarm—address imbalances early to prevent long-term damage.”
How to Improve Your Gut Microbiome
Small daily choices can reshape your gut’s microbial landscape—starting today. From your plate to your pillow, every habit plays a role in nurturing beneficial bacteria. Here’s a science-backed roadmap to optimize your inner ecosystem.
Dietary Changes for a Healthier Gut
Diversity is the cornerstone of a resilient microbiome. Aim for 30+ plant-based foods weekly—think colorful veggies, nuts, and legumes. Each type feeds different bacterial species, widening your microbial toolkit.
Prioritize these gut-loving foods:
- Fermented picks: Yogurt, kimchi, and kefir boost Lactobacilli.
- Polyphenol-rich: Dark chocolate and green tea fuel good bacteria.
- Fiber: Garlic, onions, and bananas act as prebiotics.
“A varied diet is like a buffet for your microbes—the more options, the stronger the community.”
The Role of Probiotics and Prebiotics
Probiotics introduce live strains to replenish depleted bacteria. For targeted support:
- Lactobacillus rhamnosus GG: Eases diarrhea.
- Bifidobacterium infantis: Soothes IBS symptoms.
Prebiotics (like asparagus) feed existing bacteria, helping them multiply. Pair them with probiotics for a synergistic effect.
Lifestyle Factors and Antibiotic Use
Antibiotics wipe out both harmful and beneficial bacteria. Use them only when essential, and rebuild with Bacteroides-rich foods post-treatment to lower colitis risk.
Other lifestyle tweaks:
- Stress management: Meditation improves gut motility.
- Sleep: Poor rest disrupts microbial rhythms.
| Strategy | Microbial Benefit | Example |
|---|---|---|
| High-polyphenol diet | Increases Bifidobacteria | 1 oz dark chocolate daily |
| Limit antibiotics | Preserves diversity | Use only for bacterial infections |
Conclusion
Your gut microbiome is a powerhouse, shaping everything from digestion to mood. Balancing its bacteria isn’t just about avoiding discomfort—it’s a foundation for lifelong health.
Simple changes make a big impact. Eat diverse, fiber-rich diet to feed good microbes. Prioritize sleep and stress management—they directly affect your gut. Use probiotics wisely, especially after antibiotics.
Exciting research explores microbiome therapies for chronic conditions. For personalized plans, consult a healthcare provider. Start small today—your microbiome will thank you.